
Patellar luxation (PL) is one of the most common hindlimb orthopedic pathologies seen in dogs and has been diagnosed in many other mammalian species as well. PL is the displacement of the patella out of the distal femoral patellar surface, or trochlea. The patella can displace, or luxate, medially or laterally.
Patients with PL can present with varying degrees of lameness, ranging from asymptomatic to non–weightbearing on an affected limb. Clinical signs often depend on the grade of luxation, progression of the condition and subsequent joint capsule changes, amount and frequency of exercise, and any concurrent orthopedic disruptions. Treatment options can include surgery (followed by physical rehabilitation) or conservative care that consists of pharmacologic and supplemental intervention, lifestyle changes, and physical rehabilitation.
ANATOMY
The patella is a sesamoid bone encapsulated within the patellar ligament, which itself is the distal aspect of the quadriceps femoris muscle tendon where it inserts onto the tibial tuberosity. The quadriceps femoris muscle is composed of 4 muscle group heads: the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius. These heads join in the common tendon, and all act as stifle extensors, while the rectus femoris also flexes the hip.
The extensor apparatus of the stifle includes the quadriceps femoris muscle, the patella, and the patellar ligament and its attachment on the tibial tuberosity. When the extensor apparatus is correctly aligned with the underlying axial skeleton, the patella is stable and acts as a pulley, directing the line of action for the quadriceps tendon. During neonatal and adolescent growth, normal axial alignment causes the patella to exert pressure on the articular cartilage of the trochlear groove, creating a groove with adequate depth and width as the animal grows.
Luxation of the patella can result from trauma or congenital abnormalities; congenital malformations are far more common. A congenital cause of PL is more frequent in dogs regardless of age, weight, or breed; a study from 1994 reported that 82% of the dogs in the study had congenital luxations.1 Because of the prevalent congenital nature of the disorder, breeding of patients diagnosed with atraumatic patellar luxations is strongly discouraged. Reports in the literature are conflicting about whether PL is congenital or traumatic in cats.2,3
The medical consensus is that multiple anatomic abnormalities and combinations of abnormalities can lead to PL. Common possible underlying musculoskeletal abnormalities that may contribute to PL include torsion and/or bowing of the distal femur, tibial deformity, displacement and/or atrophy of the quadriceps, femoral epiphyseal dysplasia, shallow trochlear groove with hypoplastic or absent trochlear ridges, hip dysplasia, and rotational instability of the stifle joint.4,5
GRADES OF PATELLAR LUXATION
Grade I
The patella can be manually luxated with the limb in extension, but it returns to the trochlear groove immediately when pressure is released. Flexion and extension of the joint should be normal. Spontaneous luxation of the patella during normal joint motion rarely occurs.
Grade II
The patella may be manually luxated or may spontaneously luxate with flexion of the stifle. The patella remains luxated until it spontaneously returns to the trochlear groove with active extension of the stifle or until it is manually replaced.
Grade III
Patella is continuously luxated but can easily be manually replaced. Patella does reluxate spontaneously when manual pressure is removed.
Grade IV
Patella is continuously luxated and cannot be manually reduced.
CLINICAL SIGNS
PL is graded on a scale of I to IV to differentiate the severity of clinical signs noted during physical examination. Grade I PL is commonly an incidental finding on routine examinations, with the patient presenting asymptomatically and no reported clinical indication by the owner. Dogs presenting with grade II or III luxation usually have a history of occasional skipping, intermittent or consistent hindlimb lameness, and reluctance to jump or walk down a slope. Owners may have noted hearing and/or feeling a “click” or “pop” when the dog walks or have observed that the dog will suddenly stop during a walk and look back toward the affected limb or even kick it out to the side or caudally, which reduces the luxation without further intervention. Patients with grade IV luxation often present with continual lameness or are non–weightbearing on the affected limb, with weight shifted cranially at a stance and while walking. They often cannot completely extend the affected stifle during ambulation.
Such clinical signs can vary with patient age, with mean ages at diagnosis averaging between 2 and 5 years for dogs6-8 and 37 and 40 months for cats.2,3 Signs can worsen if body weight is increased, articular cartilage damage is present, and if there is concurrent cranial cruciate ligament (CCL) rupture.9 Affected cats have shown signs of intermittent locking of the stifle after extension and can have a shuffling or crouching gait. Affected cats do not always present with lameness.2

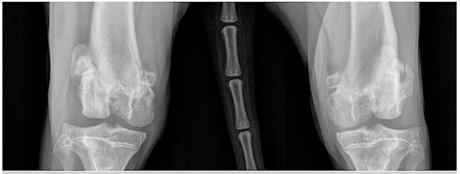
FIGURE 1. Radiographs of a 7-year-old male neutered domestic shorthaired cat that presented with chronic left hindlimb lameness. Medial patellar luxation (MPL) was diagnosed and treated conservatively until lameness worsened to grade 4/5. At the time of radiography, the patient was diagnosed with grade III MPL in the left hindlimb and grade II MPL in the right hindlimb. (A) Preoperative ventrodorsal view showing bowing of the tibia. Radiologist reported remodeling of the margin of the medial femoral trochlea on the left hindlimb. Note the medial location of the patella. (B) Preoperative mediolateral view. (C) Postoperative ventrodorsal view after a mini tightrope procedure, medial retinaculum release, and lateral fascia imbrication. CCL rupture was diagnosed during surgery. (D) Postoperative mediolateral view. Courtesy of VCA Animal Specialty Center of South Carolina, Columbia, South Carolina
DIAGNOSIS
Diagnosis of PL is primarily based on palpation of the affected stifle. Radiography can help determine the presence and degree of limb deformity and aid with planning of any surgical realignment procedures (FIGURES 1 and 2). Radiography can also determine the degree of osteoarthritis if present. On radiography, the patella will be visualized outside of the trochlear sulcus in grade III and IV PL and may be visualized within the trochlear sulcus in grade I and II luxations.4
OCCURRENCE
Medial patellar luxation (MPL) is much more common than lateral patellar luxation (LPL) in both dogs and cats, regardless of age or size of the patient. Studies have shown that MPL occurs in 83% to 95% of all dogs diagnosed with PL,10,11 whereas LPL is more common in large- and giant-breed dogs than in small-breed dogs, with a prevalence up to 33% in giant breeds.1 However, PL is most commonly diagnosed in toy and miniature breed dogs, including Chihuahuas, Maltese, miniature poodles, Pekingese, Pomeranians, and Yorkshire terriers, as well as mixed breeds5,9,12,13 and Labrador retrievers.7
Evidence of sex predilection is contradictory. Some studies show male-to-female ratios of anywhere from 1:110 to 1.8:17 to 1:1.9.5 A theory suggests that PL may be more common in male large-breed dogs and female small-breed dogs.5
On average, about 50% (range, 41% to 83%) of dogs diagnosed with MPL have bilateral luxations.14,15 In 2 studies of cats, the occurrence of bilateral PL was 38% in one3 and 81% in the other.2 Concurrent CCL disease in patients diagnosed with PL has been discussed and studied; rates range from 4% to 41%.12,16 The predominant theory behind this occurrence is that CCL ruptures or tears (commonly abbreviated as CCLRs) may result from chronic PL because of malalignment of the extensor mechanism of the stifle and internal rotation of the proximal tibia.

FIGURE 2. Radiographs of a 13-month-old female spayed Labrador retriever diagnosed with bilateral grade IV lateral patellar luxation with no CCL rupture. The patient was treated with bilateral trochlear wedge resections and tibial tuberosity transpositions, followed by physical rehabilitation. (A) Preoperative ventrodorsal view. (B) Preoperative mediolateral view of left hindlimb. (C) Preoperative mediolateral view of right hindlimb. Courtesy of Dr. Beck at Backlund Animal Clinic, Omaha, Nebraska
One study found that dogs with bilateral MPL had a higher grade of luxation in the stifle that had the concomitant CCL rupture and that “dogs with grade IV MPL were significantly more likely to have concomitant CCLR than were dogs with all other grades of luxation.”12 Conversely, researchers for another study stated that “an association between the grades of patellar luxation and CCL ruptures was not observed.”5
TREATMENT OPTIONS
Surgery
Treatment options for PL depend on the grade of luxation, any concurrent conditions (such as CCL disease), presenting signs and lameness, patient’s age, and any financial or personal limitations of the owner. Surgery is usually recommended for grade III or IV luxation; however, when it comes to recommending surgery for grade II PL, preferences vary among veterinarians, even board-certified surgeons. Some sources recommend surgery for all grade II PLs,17,18 while others recommend conservative treatment for patients with grade II luxations that present with mild and infrequent lameness and mild, nonprogressive osteoarthritis.19,20 Surgery is often recommended for puppies or young adult dogs to reduce premature wearing of the articular cartilage in the stifle joint and for patients that have active growth plates to reduce the likelihood of skeletal deformities worsening.4
1. Bone reconstruction
a. Trochleoplasty (defined as modifying the shape of the trochlear groove)
i. Trochlear wedge recession
ii. Trochlear block recession
iii. Trochlear sulcoplasty
iv. Trochlear chondroplasty in dogs younger than 6 months
v. Medial ridge elevation wedge trochleoplasty
b. Tibial tuberosity transposition
2. Soft tissue reconstruction
a. Release of retinacular tissues
i. Desmotomy
ii. Capsulectomy
b. Imbrication of retinaculum
c. Excision of redundant retinaculum
d. Antirotational sutures
e. Quadriceps release
The goal of surgery is to realign the quadriceps’ extensor apparatus, thereby stabilizing the patella in the trochlear groove to reestablish normal joint function. Doing so may minimize progression of underlying orthopedic disease, such as osteoarthritis. Most sources agree that PL surgery should involve more than one surgical correction technique to maximize the successful return of function. These techniques can broadly be divided into two classes: bone and soft tissue reconstruction. Patients with grade IV luxations will probably need multiple corrective surgeries,21 and owners should be fully informed about this likelihood. Postoperative care includes restricted activity and guided physical rehabilitation exercises to maximize healing and minimize postoperative injury or complications. After a tibial tuberosity transposition, radiography should be performed at 6 to 8 weeks to evaluate bone healing before the patient is allowed to engage in increased activity.
CONSERVATIVE MANAGEMENT
Conservative treatment for PL usually consists of pain management with analgesics and nonsteroidal anti-inflammatory drugs, as well as various nutraceuticals as prescribed by the veterinarian. Cryotherapy, or the application of cold packs, to the stifle can help provide analgesia and reduce inflammation and is easily performed at home by clients who are educated on proper application methods (below). Other physical rehabilitation modalities that focus on analgesia can be performed, such as transcutaneous electric nerve stimulation (TENS), acupuncture, laser therapy, or therapeutic ultrasound.
Cryotherapy is the therapeutic application of low temperatures. It has the following effects:
- Causes vasoconstriction, thereby decreasing blood flow
- Reduces inflammation and edema
- Decreases nerve conduction, thereby producing mild analgesia
- Decreases nerve conduction velocity, thereby reducing muscle spasm
- Decreases cellular metabolism and permeability
Cryotherapy is applied predominantly during the acute phase of inflammation; this inflammation can be caused by injury or exercise in the course of healing. Cryotherapy is particularly effective during the first 24 to 72 hours after injury/acute inflammation.
Methods of application:
- Cold packs
- Ice-water circulating compression bandages
- Ice-cup massage or ice-water immersion
- Vapocoolant spray (rarely used in veterinary medicine)
Cold packs should be malleable so they can conform to anatomic surfaces. Crushed ice in a sealed plastic bag works well. Commercially available freezer packs can be reused several times with proper sanitation and care.
Apply cold packs to the treatment area for 15 to 25 minutes at a time, with a towel or cloth between the ice pack and the patient’s skin to prevent skin damage. A wet towel will allow more rapid cooling than a dry towel. Inspect the skin every minute to ensure the tissue is not being cooled too quickly (FIGURE A).
Ice cup massage incorporates cold therapy with a light massage. It is easiest to use paper drinking cups (FIGURE B).
- Fill cups halfway or two-thirds full with water and freeze.
- Once the water is completely frozen, peel back the paper from the top of the cup to expose a half-inch to 1 inch of ice.
- Holding the cup, place the ice on the patient and make small, overlapping circles with the ice over the desired area.
- The ice will melt during treatment, so lay a towel under the patient to absorb the water.
- Be careful to avoid incisions that the veterinarian has recommended stay dry.
This method may not be possible on patients with thick coats of fur and can be difficult to perform adequately over bony/thin joints, such as the tarsus. Treatment can be performed for 10 to 25 minutes; inspect the skin as for cold pack therapy.
Cryotherapy can be used 3 to 6 times a day, ideally with at least 1 hour between treatments to allow tissue to warm back up. Continue cryotherapy daily until the injured tissue is in the subacute phase of healing. Cryotherapy can also be used after exercise to prevent or minimize reactive swelling and pain.
Contraindications to cryotherapy:
- Presence of peripheral vascular disease
- Application over areas with decreased sensation
- Open wounds
- Hypertension (cold may increase blood pressure if it is applied to the majority of the body at the same time, so avoid immersing a patient in an ice water bath if there is any history of hypertension)
- Potential for peripheral nerve injury with prolonged exposure
- History of cold hypersensitivity response/cold reaction
After pain control, conservative treatment focuses on strengthening hindlimb muscles, especially those on the opposite side of the direction of luxation. For MPLs, muscle strengthening focuses on the gluteals and biceps femoris, while for LPLs, it focuses on the sartorius and adductor muscles. Overall hindlimb strengthening can be accomplished by the following exercises (FIGURES 3 and 4):
- 3-legged and 2-legged stands
- Inclined stand
- Half-squat/sit to stand
- Full-range sit to stand
- Uphill walking
- Side stepping
- Walking on an underwater treadmill with the water level varying between stifle and mid-thigh height

FIGURE 3. (A) A 4-year-old female spayed Pomeranian displaying a compensatory stance. Note the cranial placement of the left hindlimb and mild external rotation of the right hip. This stance is caused by the patient shifting its weight to the right hindlimb to reduce weightbearing on the left. This patient was diagnosed with grade III lateral patellar luxation in the left hindlimb and grade II medial patellar luxation in the right hindlimb. (B) Patient performing incline stand with front limbs on a stable surface, therefore shifting more weight onto hindlimbs. (C) Caudal view of incline stand. Note that the patient has shifted more weight to the right hindlimb, thereby reducing weightbearing on the more symptomatic limb, the left hindlimb. (D) Patient performing 3-legged stand exercise on a balance disc. Note that therapist is supporting the patient’s trunk to prevent the patient from falling off the disc. (E) Patient standing on a BOSU ball to provide more challenge while standing on all 4 limbs and for weight-shifting exercise.

FIGURE 4. This patient is in a “half-sit” or “half-squat” posture. The therapist is using her leg as an elevated surface for the patient to sit on to perform this therapeutic exercise.
Exercises should be performed on surfaces with good traction and stability to prevent the patient from slipping. The first 4 exercises listed can be made more challenging by having the patient perform them on an unstable surface, such as a thick foam surface or on an inflated balance ball or peanut roll/physio roll.
Stretching the soft tissues on the same side of the luxation further helps in the attempt to realign the pull on the patella. The terms “passive range of motion” (PROM) and “stretching” are sometimes used interchangeably, but these are not actually the same exercise. Range of motion (ROM) exercises take the joint and soft tissues through the available range, while stretching takes the tissues beyond the normal ROM.22 When PROM is performed on a patient, the joint is held at the end range for only a few seconds; stretches are held for 15 to 30 seconds. (For some examples of PROM and stretching exercises, see this clinic resource.)
Patients being treated conservatively for PL by physical rehabilitation professionals typically go for treatment 1 to 3 times a week, with the owner performing prescribed therapeutic exercises at home daily. Treatment may continue a few months, until the patient is asymptomatic and has been reexamined by the veterinarian. If during this time the patient develops increased lameness or pain, reexamination by the veterinarian is necessary to rule out any complications, such as a CCL rupture or damage to the meniscus.
Although the primary goals of physical rehabilitation professionals treating PL patients are to decrease pain, increase flexibility of the soft tissues, increase muscle strength, and normalize gait, these professionals also need to look at the whole patient and not simply focus on the hindlimbs. Patients with PL commonly have compensatory postures (FIGURE 3), including increased cranial weight shift and increased flexion of the lumbosacral, coxofemoral, and stifle joints.23 To address compensatory patterns, trunk- and core-strengthening exercises are also warranted, as are massage and soft tissue mobilization techniques.
Postoperative Physical Rehabilitation
The general goals of physical rehabilitation are as follows:
- To return the patient and affected body part to maximum functional activity through the use of noninvasive modalities and exercises and to minimize or reverse functional impairments
- To preserve surgical interventions
- To maintain or improve quality of life
- To prevent future injury
- To educate clients
After surgery to correct PL, the goals of a physical rehabilitation program change as the patient progresses through each phase of tissue healing: the inflammatory phase, the reparative phase, and the remodeling/maturation phase.22
Inflammatory Phase
The inflammatory phase occurs during the first 3 to 5 days after injury or surgery and is characterized by an acute vascular response focused on hemostasis of the surgical site. It is also characterized by a cellular reaction focused on the use of neutrophils and macrophages to “clean up” the site through debridement, phagocytosis, matrix synthesis, and cell recruitment and activation. During the first week after surgery, cryotherapy is used to reduce inflammation. The patient’s activity should be restricted to slow leash walks lasting 5 to 8 minutes for elimination purposes 3 to 4 times a day. Patients should be prevented from running, jumping, playing, and having access to stairs.
Gentle PROM exercises should be performed on the stifle and hip, putting them through gentle flexion and extension to maintain flexibility, prevent adhesion formation between soft tissues, and help maintain joint capsule health. PROM exercises should be performed 3 to 4 times a day, for 5 to 10 repetitions on each joint. Massage of the quadriceps, hamstrings, and gluteal muscles before PROM helps warm up the tissues and can aid in relaxation and analgesia; massage can be performed for 5 to 15 minutes 3 to 4 times a day.
Reparative Phase
The reparative phase occurs within 3 to 14 days after injury and is characterized by the cellular response of fibroblasts and endothelial cells. The fibroblasts synthesize collagen and create new extracellular matrix components. The endothelial cells work to form new capillaries and help produce granulation tissue. During weeks 2 and 3, cryotherapy can be discontinued or applied only as needed, and the use of warm packs can be started. Warm packs can be wrapped around the stifle and held in place for 10 to 15 minutes 2 to 3 times a day before activity, massage, or PROM exercises. Massage and PROM exercises as performed in week 1 should be continued.
Patients may begin static weight-shifting exercises (wherein the patient is not being asked to move limbs during the exercise), which can include 3-legged stands and assisted standing on a balance board. Activity restriction should be continued, and it is recommended that all therapeutic exercises be performed while motion is limited to the sagittal plane only.22 After suture removal and recheck by the veterinarian 10 to 14 days after surgery, the veterinarian may recommend increasing leash walks by an additional 5 to 10 minutes as tolerated by the patient.
Remodeling Phase
The remodeling phase occurs 2 to 3 weeks after injury, with tissue strength continuing to increase over the course of 1 year. This phase is characterized by remodeling of collagen fibers to orient in parallel to lines of stress as well as becoming crosslinked, thereby strengthening the healing tissue. This is the phase in which scar tissue is formed.
Ideally, the patient will be consistently placing partial weight on the surgical limb by the end of 2 weeks. For 3 to 8 weeks after surgery, therapeutic exercises will continue to be added and modified, with the goals of maintaining or gaining normal ROM of the stifle, increasing weightbearing of the surgical limb, and building muscle strength of the hindlimbs and core stabilizers. After a examination by a veterinarian and stifle radiography at 6 to 8 weeks after surgery, the physical rehabilitation professional will likely modify the patient’s exercise program to include more challenging exercises and increase walks with the goal of returning to full activity.
PROGNOSIS AND COMPLICATIONS
Overall prognosis for surgically corrected PLs is good to excellent. The most common complications are patellar reluxation, implant complications (ie, pin migration), tibial tuberosity fracture avulsion, and wound dehiscence. Overall postoperative complication rates range from 17% to 51%.10,11 It has been theorized that increased body weight is a risk factor for postoperative complications7; higher grades of luxation are also at higher risk. The prognosis for long-term outcome among PL patients in general, regardless of treatment option, worsens the older the patient is at onset and as the grade of luxation and severity of clinical signs increase.17
To my knowledge, no major studies have assessed whether outcomes differ substantially between PL patients treated conservatively with physical rehabilitation and those treated surgically; most studies focus on surgical techniques and outcomes. Gibbons et al did report that the “long-term outcome for dogs with grade 1 and 2 patellar luxations treated non-surgically was less favourable than that for dogs treated surgically.”7 Thirty-three percent of the limbs included in that study were treated nonsurgically. Of these, 86% had excellent to good outcome and 14% had fair or poor outcome. However, the study did not elucidate the treatment parameters for patients treated nonsurgically. Loughin et al found that 47% of their feline patients that were treated nonsurgically had excellent outcome.2 They stated that “lameness may not be a good indicator of the need for surgical correction and it seems prudent to recommend a period of nonsurgical management (rest and analgesics) prior to surgical intervention, particularly in cats in which signs of lameness have been present for < 2 months.”2
Environmental changes at home can help patients recover from surgery and help reduce chances of further injury on non–surgically repaired limbs. Clients should be encouraged to keep the pet’s nails well trimmed and clip any long interdigital fur from the bottom of the paws to maximize traction while walking. Clients who have only wood, linoleum, or other slick flooring at home can be instructed to lay out rubber-backed throw rugs or yoga mats to help prevent their pet from slipping. Blocking access to stairs and couches or beds that the pet is used to jumping onto should be discouraged. Having overweight or obese patients lose weight before surgery or even after surgical recovery is an excellent lifestyle change that increases life expectancy and reduces the negative effects of osteoarthritis.24
CONCLUSION
Patellar luxation is a common orthopedic condition diagnosed in dogs. It is more common in toy and small breeds, with the patella more likely to luxate medially. Physical rehabilitation can play an important role in helping patients recover after surgical correction and can be a realistic option for patients that are not surgical candidates. Physical rehabilitation after surgical correction for PL attenuates muscle atrophy and significantly improves weightbearing by 8 weeks after surgery.25
When tailoring a physical rehabilitation program to the needs of a specific PL patient, physical rehabilitation professionals must consider any surgical interventions the patient has received. Patients that have had bony reconstruction corrective techniques are usually treated with more conservative, low-impact therapeutic exercises during the first 6 to 8 weeks of postoperative recovery to minimize the possibility of hardware migration, avulsions, or fractures. Concurrent CCL rupture or hip dysplasia may alter the recommended rehabilitation exercise program and add challenges to the program.
Veterinary technicians and nurses should also be familiar with surgical interventions performed on their patients and be able to answer clients’ general questions regarding the initial recovery period in the hospital and after discharge. Clients should be encouraged to seek a consultation with a certified physical rehabilitation provider to maximize their pet’s recovery and return to function, as well as to minimize any potential complications after a PL surgical repair. Veterinary technicians and nurses should be proficient in describing the activity restrictions prescribed by the veterinary surgeon and educate their clients in different lifestyle changes that can beneficial for their pet.
Author: Maria Maddox, LVT, CCRP, AMCP
Link & References: https://todaysveterinarynurse.com/articles/luxating-patellas-pathology-and-treatment-options/
Need rehab help for your dog or cat? Meet virtually with our Consultant Experts Here – right in the comfort of your own home.